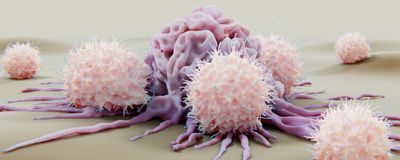
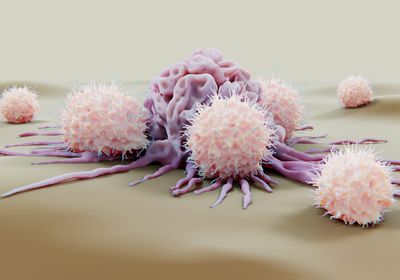
ABOVE: NK cells attack cancer cells, but if they turn into intILC1, they become powerless against a tumor. ©istock, selvanegra
When a rogue cell starts proliferating out of control, the first responders on the scene should be the body’s own immune cells—for example, natural killer (NK) cells, which use toxic molecules to dissolve foreign cells. Ideally, proteins that are specific to cancer cells would trigger the immune cells to destroy the cancer cells, and a growing category of new NK cell therapies harness these cellular assassins to fight cancer.
However, cancers have evolved creative strategies to evade these cellular sentinels. One way they do this is by turning cells that are typically cancer assassins into docile bystanders. For example, a 2017 study showed that tumors can avoid being killed by triggering the release of transforming growth factor beta (TGFb), a molecule that can turn NK cells into intermediate type 1 innate lymphoid cells (intILC1).1 This immune cell type is much less effective against tumors, which can undermine immunotherapy efforts.
“Tumors have developed these fantastic environments to survive,” said Sebastian Scheer, an immunologist at the Luxembourg Institute of Health and coauthor of the study. But that environment is not the only way for NK cells to transform into intILC1. In a new study in Cell Reports, a team at Monash University led by Scheer found that the molecule disruptor of telomeric silencing 1-like histone lysine methyltransferase (DOT1L) plays an important role in maintaining NK cell functions.2 When DOT1L levels decline, the NK cells turn into benign intILC1 even in the absence of cancer-induced TGFb.
Changing a cell’s functions so drastically often requires changing its genetic programming, so the team investigated DOT1L, an epigenetic modifier that changes cells’ epigenetic marks. DOT1L seemed to shape the unique way that NK cells read their genome.
When the researchers deleted DOT1L from mature NK cells in the new study, it became clear that deleting just this one protein was enough to change the levels of genes and proteins expressed in the cell, including those of a transcription factor called myocyte enhancer factor 2C (MEF2C) that was previously linked to NK cell function.3 As a result, some of the NK cells turned into intILC1, despite not being near tumors or exposed to TGFb.
“It was really quite surprising that this process would happen in normal, healthy mice when you remove one epigenetic regulator,” said Nicholas Huntington, a cancer immunologist at Monash University who co-authored this study. “We had only ever observed this phenotype in highly immunosuppressed solid tumors.”
Eric Vivier, an immunologist at Aix-Marseille University who was not involved in the study, said this work fills in some of the gaps in scientists’ understanding of how NK cells might turn into intILC1. However, he suspects DOT1L is not the only protein in play. “It would be very surprising if DOT1L by itself is both necessary and sufficient for this transition,” he said. “There will be many more mechanisms to dissect.”
To Huntington, this new path to quelling NK cells is especially concerning because some cancer therapies inactivate DOT1L. “It’s a cautionary tale,” he said. If DOT1L inhibitors were used in conjunction with an NK cell therapy, such as NK cells with chimeric antigen receptors or molecules that attract NK cells to tumors, the combination could render the therapy impotent.
“You might be differentiating NK cells into useless intILC1 and then trying to target those with a therapeutic,” Huntington said. “They won't work.” Instead, he thinks his team’s findings can point to the importance of investigating ways to maintain DOT1L levels in NK cells when designing NK cell-based cancer treatments.
For example, Vivier’s biotech company Innate Pharma is developing therapies that use specialized immune proteins to marshal NK cells to attack tumors.4 The discovery of DOT1L’s role in NK cell function has made him think about how it might impact these drugs’ effectiveness. “It prompts us to investigate whether treatments that have been designed to harness NK cells can actually bypass this transition between NK cells and ILC1-like cells,” he said.
Although maintaining DOT1L levels might not be feasible, Scheer is currently investigating the role that MEF2C and other transcription factors may play in NK cell function to search for better drug targets.
“This information potentially guides drug developers to start thinking about some of the vulnerabilities of NK cells in a tumor microenvironment and how to potentially overcome some of these hurdles to effective immunity,” Huntington said.
References
1. Gao Y, et al. Tumor immunoevasion by the conversion of effector NK cells into type 1 innate lymphoid cells. Nat Immunol. 2017;18(9):1004-1015.
2. Sudholz H, et al. DOT1L maintains NK cell phenotype and function for optimal tumor control. Cell Rep. 2024;43(6):114333.
3. Li JH, et al. MEF2C regulates NK cell effector functions through control of lipid metabolism. Nat Immunol. 2024;25(5):778-789.
4. Gauthier L, et al. Control of acute myeloid leukemia by a trifunctional NKp46-CD16a-NK cell engager targeting CD123. Nat Biotechnol. 2023;41(9):1296-1306.