Stay up to date on the latest science with Brush Up Summaries.
Precision Medicine in Cancer
Precision medicine for cancer treatment involves tailoring treatments to an individual patient’s genetics and lifestyle, as well as the cellular and molecular features of their tumor and its microenvironment.1 Scientists and clinicians often refer to precision medicine as personalized medicine, individualized medicine, or targeted therapy. Precision medicine is a key alternative to current standard treatments such as chemotherapy and radiation, which are only effective in a subset of patients and are toxic to healthy tissues as well as cancer cells.2
Cancer is an extremely heterogeneous disease; there are hundreds of different types of cancers, many of which have subtypes based on their molecular features.2 Clinicians use precision medicine to identify which therapies will be effective for individual patients by analyzing the genetic mutations that drive tumorigenesis or other molecular features of the tumor, for example via next generation sequencing.3
When Is Precision Medicine Used for Cancer Treatment?
Physicians may use precision medicine in oncology when a tumor fails to respond to current standard treatments, such as chemotherapy and radiation. They can sequence the tumor’s genome to identify genetic mutations that drive tumor growth or contribute to treatment resistance, and then use this information to match the tumor to a suitable treatment.3
Doctors also use precision medicine to assess a person’s risk of developing cancer. For example, if a person has a known family history of cancer, genome sequencing can determine if they carry an inherited mutation that puts them at high risk of developing cancer in the future. People with a high risk can be tested for signs of cancer regularly and treated at earlier stages of disease for better prognosis.4
Table 1: Examples of precision medicine in oncology, including the biomarker or gene they target and the relevant cancer type.
| Treatment | Target | Cancer Type |
| Imatinib5 | BCR—ABL1 fusion oncogene | Chronic myeloid leukemia |
| PARP inhibitors (olaparib, rucaparib, niroparib, talazoparib)6 | BRCA1 and BRCA2 mutations | Breast cancer, among others |
| Pembrolizumab, nivolumab7 | Lynch syndrome genes (germline mismatch repair variants) | Colorectal and endometrial cancers |
| Trastuzumab8 | HER2/neu ERBB2 | Breast cancer |
| BRAF inhibitors9 | BRAF V600E | Metastatic melanoma |
Examples of Precision Medicine in Cancer
Personalized treatments for specific cancer mutations
The first major example of precision cancer medicine was in the treatment of chronic myeloid leukemia (CML). The major driver of CML is a fusion oncogene known as BCR-ABL, which is the result of a chromosomal translocation.5 In the late 1990s, scientists developed a drug called imatinib that inhibits the resulting fusion protein, leading to drastically improved clinical outcomes; it is now typically the first line of treatment for patients with CML rather than chemotherapy.9 Researchers have since identified many other mutations and targeted treatments for different cancer types.
Biomarkers for cancer diagnosis, treatment efficacy, and resistance
Clinicians can now diagnose cancer, perform molecular tumor profiling, assess cancer treatment efficacy, and monitor disease progression and tumor burden using cell-free DNA (cfDNA) testing, which is another form of personalized medicine.10 Using a procedure known as a liquid biopsy, doctors collect the circulating tumor DNA (ctDNA) found in the peripheral blood of a patient and analyze the sample with a blood test, eliminating the need for invasive tissue biopsy techniques.11
See Also “The Basics and Applications of Cell-Free DNA”
Scientists also use precision medicine in cancer therapy to find biomarkers of treatment resistance. For example, intrinsic and acquired resistance to chemotherapy is common in patients with triple negative breast cancer (TNBC) and represents a major hurdle in the successful treatment of this disease.12 There are now several biomarkers that can predict the resistance of TNBC tumors to chemotherapy, helping inform better treatment options.12 Similar biomarkers for resistance to radiation therapy are emerging.13
Precision medicine in cancer immunotherapy
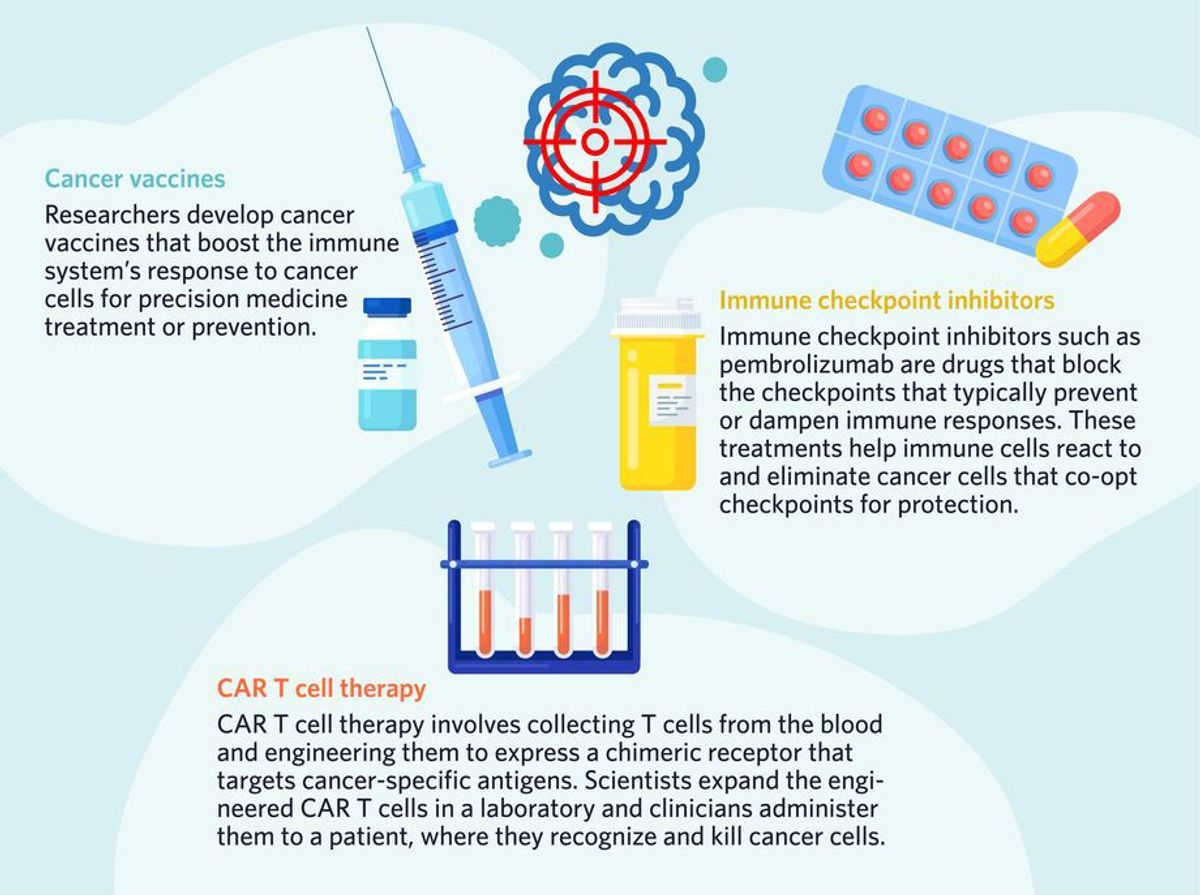
Another way that scientists harness the power of precision medicine in cancer treatment is through targeted immunotherapy. Chimeric antigen receptor (CAR) T cell therapy involves collecting T cells from a patient or healthy donor and engineering them to express a receptor that targets unique and specific antigens expressed on different cancer cells.14 The engineered T cells are then expanded and infused back into the patient, where they recognize and kill cancer cells more effectively.14
See Also “The Basics of the Tumor Microenvironment”
Other precision medicine immunotherapies include cancer vaccines and monoclonal antibodies, such as pembrolizumab. This drug is an immune checkpoint inhibitor that targets programmed death protein 1 (PD-1), which is expressed by immune cells, and its ligand, programmed death ligand 1 (PD-L1), which is expressed by some cancer cells.15 Cancer cells often hijack the PD-1/PD-L1 pathway to evade the immune system; by upregulating their surface expression of PD-L1, cancer cells trigger immune exhaustion within the tumor microenvironment. Pembrolizumab blocks PD-1 to prevent this.16 Clinicians also use PD-1 itself as a biomarker in precision medicine to identify patients who would benefit from this type of treatment.15

- Habeeb NW-A, et al. The use of targeted therapies for precision medicine in oncology. Clin Chem. 2016;62(12):1556-1564.
- Krzyszczyk P, et al. The growing role of precision and personalized medicine for cancer treatment. Technology. 2018;6(3-4):79-100.
- Morash M, et al. The role of next-generation sequencing in precision medicine: a review of outcomes in oncology. J Pers Med. 2018;8(3).
- Yang J, et al. An overview of the use of precision population medicine in cancer care: first of a series. Cureus. 2023;15(4):e37889.
- Iqbal N, Iqbal N. Imatinib: a breakthrough of targeted therapy in cancer. Chemother Res Pract. 2014;2014:357027.
- Imyanitov EN. Cytotoxic and targeted therapy for BRCA1/2-driven cancers. Hered Cancer Clin Pract. 2021;19(1):36.
- Yurgelun MB, Hampel H. Recent advances in Lynch syndrome: diagnosis, treatment, and cancer prevention. Am Soc Clin Oncol Educ B. 2018;(38):101-109.
- Wang J, Xu B. Targeted therapeutic options and future perspectives for HER2-positive breast cancer. Signal Transduct Target Ther. 2019;4(1):34.
- Schwartzberg L, et al. Precision oncology: who, how, what, when, and when not? Am Soc Clin Oncol Educ B. 2017;(37):160-169.
- Wan JCM, et al. Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer. 2017;17(4):223-238.
- Mouliere F, et al. Multi-marker analysis of circulating cell-free DNA toward personalized medicine for colorectal cancer. Mol Oncol. 2014;8(5):927-941.
- Ferrari P, et al. Molecular mechanisms, biomarkers and emerging therapies for chemotherapy resistant TNBC. Int J Mol Sci. 2022;23(3).
- Baumann M, et al. Radiation oncology in the era of precision medicine. Nat Rev Cancer. 2016;16(4):234-249.
- Chen L, et al. CAR-T cell therapy for lung cancer: Potential and perspective. Thorac cancer. 2022;13(7):889-899.
- Liu X, Cho WC. Precision medicine in immune checkpoint blockade therapy for non-small cell lung cancer. Clin Transl Med. 2017;6(1):7.
- Collins LHC, Moutasim KA. Current concepts in PD-L1 testing in head and neck squamous cell carcinoma: overview, developments and challenges. Diagnostic Histopathol. 2023;29(4):225-231.
